Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care. Your progress notes should include evidence of a mental health diagnosis, describe symptom impact on functioning, and show how your interventions address the treatment plan goals. Accurate and thorough documentation is the backbone of successful behavioral health billing.
Substance Use Disorder (SUD) Treatment

Mental health care providers are essential to ensure emotional wellbeing. The services and coverings offered by the providers span several critical elements to ensure a smooth and efficient process. However, mental health billing mental health billing for dummies for psychologists is often a hindrance to the treatment procedure if there are lapses on the part of the billing system. This might result in incorrect or inadequate documentation and issues with pre-authorization. A few issues and myriad other factors could make it difficult for mental health professionals to manage their practices effectively.
Chapter 4: EOB & Claims Processing
Make sure that you are aware of your patient’s insurance plans and benefits before making a claim. Although this sounds like a huge job, in the long run, making sure you know the coverage available for each patient before they receive any services will be very beneficial in the long run. To know what coverage your patients have, it’s best to verify benefits (VOB) for each patient before you provide any services. A VOB checks the patient’s policy regarding the service they are visiting for and gives providers information that is not available from a patient’s insurance number. Mental healthcare practitioners should only ever use ICD-10 codes to bill for mental health claims. Remember, the DSM-IV is used by all mental healthcare practitioners to help in the diagnosis of clients/patients with mental health ailments.

A Complete Guide To Mental Health Billing
We’ve provided a quick list of the mistakes, and if you need any further information about them, be sure to check out this website for further explanation. The psychiatric diagnostic evaluation, also known as a psych evaluation, is typically performed to evaluate patient’s medical and psychiatry mental health. The patient’s behavior, thought process, cognitive skills etc will be examined, and provider will devise a treatment plan based on the patient’s readiness and capacity to react to treatment.
A clearinghouse is usually a service offered by a third-party organization that acts as a central repository and middle-man to your claim submission process. Anyway, this section lists the industry terms used within bookkeeping mental health billing. After all, there are differences between the types of claims that hospitals submit compared to those coming from mental health facilities.

At the time that was an all-time high and the http://midcanadaminigroup.ca/2021/03/29/8-best-online-small-business-bookkeeping-services/ survey that that statistic came from suggested that denial rates weren’t slowing down. The right billing partner can save thousands in lost reimbursements and labor. Only 1 in 500 claims ever gets appealed—yet 44% of appeals are successful.
- Eligibility checking also falls under the category of must-have reporting features.
- The financial stability of your firm depends on mental health billing, which is more than just administrative work.
- If the insurance company has a preferred filing method, make sure you comply with it and the time frame set forth by the insurer.
- We recommend reading and using Barbara Griswald’s book Navigating the Insurance Maze as a primer on how to submit paper claims correctly.
- Underbilling by choosing instead could leave significant revenue on the table.
If your claim looks right, the clearinghouse sends the claim directly to the insurance company you have selected. For mental health providers, the billing process can be challenging but not impossible. If you dig into the points mentioned in this article, you will get where you want to be – having your practice receive the deserving reimbursements on time. During this approach, practices can look up details about your patient’s coverage that aren’t frequently listed on the insurance card. Even though many patients possess active coverage, the services might not be reimbursed as a benefit, so this step is essential to make mental health billing smoother.
- The odds of obtaining that payment shrink once your patient has left the facility.
- Use a calendar or EHR alerts to track authorization dates and visit limits to avoid claim rejections or missed revenue.
- When incorrect information or typos sneak into the initial patient records, those mistakes will appear on every bill until you realize there’s a problem.
- ICANotes offers full-service behavioral health Revenue Cycle Management (RCM) to support your practice every step of the way — from eligibility verification to payment posting.
- Ideally, your patient portal will be able to store patients’ credit card information for easy, one-click payments.
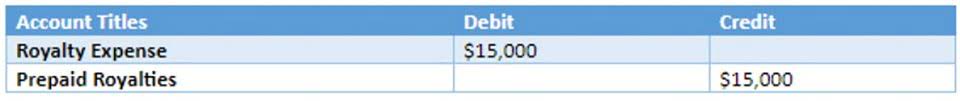
Smart prompts and structured note formats help reduce omissions and improve claim acceptance rates. Efficient handling of denials prevents revenue loss and ensures you receive fair payment for your services. The majority of group practices and almost all successful individual private practices utilize outside billing services in one capacity or another. Call the same company using the same eligibility and benefits number and ask for claims processing and EOB accounting. Again, if you’re tired reading about the ins and outs of insurance billing, you might save time, money, and headache delegating this part of your private practice. You are to charge them after the fact for their patient responsibility payment per session as listed on the completed EOB your receive from filing your claims.
Filing claims involves submitting each date of service with all this information one by one. Each insurance company has their own online portal to submit claims, some terrible, some fairly okay. This is the standardized form that insurance companies accept (although now less than before) for your claims submission. Normally all of this information gets submitted digitally, rendering this form useless, unless you know exactly how to fill it out.